Reduce HbA1c, Reduce Complications
To keep blood glucose levels in the target range and to reduce the risk of complications, accurate doses of insulin need to be delivered to the body. Different therapies can include:
-
Conventional Therapy
2 to 3 injections per day of mixed long- and short-acting insulin.
-
Multiple Daily Injections (MDI)
3 or more injections with rapid-acting insulin and 1 to 2 injections with long-acting insulin per day.
-
Insulin Pump Therapy
Insulin pump therapy replaces the need for frequent injections by delivering rapid-acting insulin 24 hours a day. A programmed insulin rate mimics the basal (background) insulin production by the pancreas and can be better adjusted to the body's needs. Rapid-acting insulin acts very quickly to help minimise variations in blood glucose levels in response to carbohydrate intake or, if needed, to lower high blood glucose values.
MONITORING BLOOD GLUCOSE
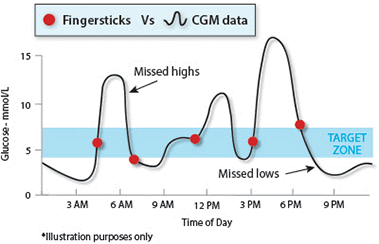
When you monitor your blood glucose with a fingerstick test, you measure it at the moment you perform the test. To get an even better picture of how well you're managing your diabetes, it is important to look at your average blood glucose levels over a few months.
The test used to work this out is the haemoglobin A1c (HbA1c) test. HbA1c is a kind of chemical 'footprint' that shows how much glucose has been in your bloodstream over the past 60 to 90 days (the average lifespan of a red blood cell). Research shows that, for people living with diabetes, an HbA1c level of ≤ 7 greatly reduces the risk of long-term complications1,2.
Whether you use an insulin pump or injections, it's important to have your HbA1c levels tested at least every three months by your doctor, endocrinologist or diabetes educator. That way you can get a clearer picture of how well you're doing and make the necessary treatment and lifestyle adjustments to do even better.

Continuous Glucose Monitoring
When you take BG tests to look at your glucose values you will likely be asked to take 5-10 readings per day. This provides several snapshots as to what your glucose values are at that time, but it does not give information as to whether your glucose levels are going up or down. Continuous Glucose Monitoring consists of a small device which contains a small electrode that sits under the skin and will take a glucose reading up to every five minutes (288 per day) and send those individual readings as well as a graph of our previous readings to your pump or phone. This allows you to see not only your current glucose reading but also what it looked like earlier in the day and will also let you know if your glucose values are currently going up or down.
Seven Steps for Glucose Control
Better blood glucose control has gained significant attention since the release of the landmark Diabetes Control and Complications Trials (DCCT). The study emphasised the importance of good control in helping patients feel better, and ultimately enjoy a better lifestyle. Here are seven steps that will help you gain greater control of your diabetes management:
2
Treating Hypoglycaemia (Low Blood Glucose)
Your healthcare professionals will provide specific guidance for you to treat hypoglycaemia. General guidelines suggest:
It is important to establish a routine for when your blood glucose is low. Have something available to treat a low and you are less likely to over treat and raise your glucose levels too much.
3
Treating Hyperglycaemia (High Blood Glucose)
Your healthcare professionals will provide specific guidance for you to treat hyperglycaemia. General guidelines suggest:
High blood glucose can occur while using the pump for the same reasons it did when you were not on the pump, including some situations that are unique to insulin pump therapy:
- Too much food
- Not enough insulin
- Loss of insulin potency
- Not receiving insulin from the pump
The goal of treating hyperglycaemia is to prevent Diabetic Ketoacidosis (DKA) and delay or prevent diabetes complications due to high blood glucose over an extended period of time.
4
Sick Day Management
Illness and infection put extra stress on the body and often raise blood glucose3. An insulin pump allows you to make adjustments to quickly and easily respond to illness and infection. Your healthcare professional will provide specific advice to you on how to manage on days where you are sick. General Guidelines for sick day management include3:
- Checking blood glucose levels every 2 hours
- Checking urine for ketones
Notify your healthcare professional if you have moderate or high ketones, nausea, vomiting, or if your glucose levels remain high. Keep a few supplies on hand in case you become sick. Recommended items include: - Sugar-free liquids (e.g. broth) can be used to replace lost fluids and prevent dehydration
- Fluids that contain sugar can be used to replace needed calories if you are unable to eat
- Extra glucose meter strips
- Ketone strips
- Medications (sugar-free) for cough, congestion, nausea or vomiting, and fever.
6
7
Managing Infusion Sites
If you are using an insulin pump, it is important to be proactive about keeping your infusion set healthy and your insulin, reservoir, and infusion set fresh. With a little care, you can take full advantage of the benefits of insulin pump therapy and avoid serious problems.
A few simple principles can significantly improve your results:
- Change/rotate infusion site regularly
- Inspect infusion site frequently
- Use appropriate sites
- Keep adequate supplies on hand
You may be interested in
REDUCING LONG TERM COMPLICATIONS
See how you can safeguard your future and avoid long term complications.
More DetailsCONTINUOUS GLUCOSE MONITORING
Monitor your glucose levels 24/7 with the accuracy of Enlite Sensors.
More Details- The Diabetes Control and Complications Trial (DCCT) Research Group. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. NEJM. 1993;329(14):977-986.
- The Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications (DCCT/EDIC) Study Research Group. Intensive diabetes treatment and cardiovascular disease in patients with Insulin Dependant Diabetes. NEJM.2005;353(25):2643-2653.3.Diabetes Australia. (2016).Managing sick days for Type 1 diabetes.Available at: https://static.diabetesaustralia.com.au/s/fileassets/diabetes-australia/89f49125-e2e9-4233-868e-c8fe46d99b4e.pdf.